Cell Phone Radiation Damages Sperm, Studies Show
Phones Carried on Belt or in Pant’s Pocket May Harm Reproductive Health
Although most scientific and public attention on the issue of the safety of cell phone radiation has focused on evidence suggesting an increased risk of brain tumors (Baan 2011), a little-noticed but growing body of research points to a new concern – sperm damage (La Vignera 2012).
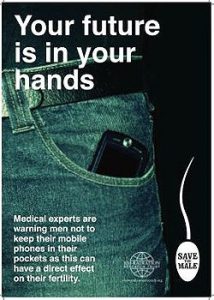
In a comprehensive review of the published scientific literature, the Environmental Working Group found ten human studies that have identified a startling variety of changes in sperm exposed to cell phone radiation. In the most striking findings, men who carried their phones in a pocket or on their belts were likelier to have lower sperm counts and/or more inactive or less mobile sperm. These findings accord with similar results in laboratory animals.
Collectively, the research indicates that exposure to cell phone radiation may lead to decreases in sperm count, sperm motility, and vitality, as well as increases in indicators of sperm damage such as higher levels of reactive oxygen species (chemically reactive molecules containing oxygen), oxidative stress, DNA damage and changes in sperm morphology (see summary below).
Many men who talk on a cell phone using Bluetooth or other headsets keep the phone in a pants pocket or clipped to a holster. This exposes their reproductive organs to cell phone radiation, and several studies have found lower sperm count and/or poorer sperm quality in men who use their phones this way than in those who do not.
Scientists have yet to identify a mechanism by which cell phone use might cause such effects (Makker 2009). However, the research appears to rule out the possibility that the changes are caused by simple heating, which is considered a possible source of some radiofrequency radiation-related health problems (De Iuliis 2009; Volkow 2011).
The findings are particularly significant because infertility affects approximately 15 percent of couples of reproductive age, and nearly half of these cases are linked to male fertility (Sharlip 2002). The number and consistency of the findings raise the possibility that cell phone radiation could contribute to this significant public health problem and demand further investigation.
Studies linking cell phone exposure to harmful effects on sperm have been done in the United States, Australia, Austria, Hungary, Poland, Turkey, and South Africa, using diverse methodologies. Some scientists compared sperm counts and sperm health in men who wore cell phones on the hip with those who carried them elsewhere on the body or did not use cell phones at all. In others, researchers exposed sperm to cell phone radiation under laboratory conditions. In still others, scientists examined whether there was a correlation between sperm health and the intensity of cell phone use among men undergoing evaluation for infertility.
Among the findings:
- Men who carried a phone in a hip pocket or on the belt had 11 percent fewer mobile sperm than men who kept a phone elsewhere on the body (Kilgallon 2005).
- Men who carried a cell phone on the belt and used it intensively during a five-day test period had a 19 percent drop in highly motile sperm from their previous levels (Davoudi 2002).
- Men who talked on the phone for more than an hour a day had 17 percent fewer highly motile sperm than men who talked less than 15 minutes a day (Fejes 2005).
Laboratory studies on the effects of cell phone radiation on rats, rabbits, and other animals have found similar effects on reproductive health (Kesari 2011; Mailankot 2009).
All these studies found statistically significant correlations between cell phone radiation and sperm health, and many found that the adverse changes increased with the amount of radiation exposure. Opinions differ on the possible mechanism by which cell phone radiation might produce these changes (Falzone 2010).
Several research papers include unambiguous statements on the potential of cell phone radiation to affect men’s reproductive health:
- “Keeping the cell phone in a trouser pocket in talk mode may negatively affect spermatozoa and impair male fertility” (Agarwal 2009).
- “Use of cell phones decreases the semen quality in men by decreasing the sperm count, motility, viability, and normal morphology. The decrease in sperm parameters depended on the duration of daily exposure to cell phones and independent of the initial semen quality” (Agarwal 2008).
- “These findings have clear implications for the safety of extensive mobile phone use by males of reproductive age, potentially affecting both their fertility and the health and wellbeing of their offspring” (De Iuliis 2009).
- “Overall, these findings raise several related health policies and patient management issues that deserve our immediate attention. Specifically, we recommend that men of reproductive age who engage in high levels of mobile phone use do not keep their phones in receiving mode below waist level” (De Iuliis 2009).
- “Our results showed that cell phone use negatively affects sperm quality in men… Men with poor sperm quality planning for pregnancy should be advised not to use cell phones extensively” (Gutschi 2011).
- “The results show that human spermatozoa exposed to RF-EMR have decreased motility, morphometric abnormalities, and increased oxidative stress, whereas men using mobile phones have decreased sperm concentration, motility…, normal morphology, and viability. These abnormalities seem to be directly related to the length of mobile phone use” (La Vignera 2012).
Given the backdrop of increasing infertility rates (Swan 2006), the research findings should be a wake-up call to male cell phone users who are trying to have children or may want to in the future.
Even as scientists continue to gather new data on health risks from cell phone radiation, the findings underscore that consumers should practice simple, precautionary safe-cell-phone-use habits, such as keeping the phone away from the body, to protect their health and fertility. Men, in particular, should avoid carrying a cell phone on the belt or in a pants pocket when in use.
What About Women’s Health?
There are no published studies examining cell phone radiation’s effect on women’s reproductive health. Such studies are much more difficult to carry out since they often require invasive techniques. However, several recent articles suggested cell phone radiation might harm the developing fetus. For example, a 2009 study in Turkey found that after pregnant rats were exposed to cell phone radiation for 15 minutes twice a day during the entire gestation period, their female pups had fewer ovarian follicles (Gul 2009). A 2012 study by Yale University School of Medicine researchers found that mice exposed to cell phone radiation during gestation were hyperactive and had impaired memory (Aldad 2012).
There have been similar findings in two human studies. UCLA researchers reported that cell phone exposure during pregnancy and after birth was associated with behavioral problems in young children (Divan 2008; Divan 2012). This line of research is just beginning, but a recent review article emphasized that cell phone radiation might impact reproduction and development in both men and women (Merhi 2011).
Table: Peer-reviewed studies of the effects of cell phone radiation on male reproduction
| Reference | Study design | Finding | Type of exposure |
|---|---|---|---|
| Davoudi M, Brossner C, Kuber W. 2002. The influence of electromagnetic waves on sperm motility. Journal für Urologie und Urogynäkologie 19: 19-22. | Semen analysis for 13 male volunteers who carried a cell phone on the belt and actively used it for five days. | Compared to a period of cell phone use on the belt by the same volunteers, cell phone use was associated with decreased sperm motility. The percentage of highly motile sperm (classified as “rapid progressive sperm”) dropped from a mean of 32% to a mean of 26% after the exposure. | GSM phone; study participants used phones for at least 6 hours/day. |
| Fejes I, Zavaczki Z, Szollosi J, Koloszar S, Daru J, Kovacs L, et al. 2005. Is there a relationship between cell phone use and semen quality? Arch Androl 51(5): 385-93. | Semen analysis for 371 men who attended an infertility clinic in 2002-2004. | Low-volume cell phone users (less than 15 minutes a day) had a higher percentage of rapid progressive motile sperm (48.7%) than high-volume (more than one hour a day) cell phone users (40.6%). | The pattern of use identified by a questionnaire, including duration of phone possession and frequency of daily use. |
| Kilgallon SJ, Simmons LW. 2005. Image content influences men’s semen quality. Biol Lett 1(3): 253-5. | Analysis of sperm samples from 52 healthy men aged 18-35. | Men who carried a cell phone in a hip pocket or on the belt had lower sperm motility (49.3% motile sperm) than men who did not use a cell phone near the hip (55.4% motile sperm). | Questionnaire responses identified men who carried a cell phone in a hip pocket or on the belt, non-users, and those who kept a phone elsewhere. |
| Erogul O, Oztas E, Yildirim I, Kir T, Aydur E, Komesli G, et al. 2006. Effects of electromagnetic radiation from a cellular phone on human sperm motility: an in vitro study. Arch Med Res 37(7): 840-3. | Semen samples were collected from 27 men exposed to cell phone radiation under laboratory conditions. | Exposed specimens had a decrease in rapid progressive sperm from 13% to 9%, a decrease in slow progressive sperm from 44% to 34%, and an increase in immotile sperm from 36% to 51%. | Test specimens were exposed for 5 minutes to GSM cell phone radiation at 900 MHz. |
| Wdowiak A, Wdowiak L, Wiktor H. 2007. Evaluation of the effect of using mobile phones on male fertility. Ann Agric Environ Med 14(1): 169-72. | Sperm parameters were examined in a group of 304 males enrolled at an infertility clinic in 2004-2006. | 16.7% of regular cell phone users had normal semen morphology, compared to 55.6% of non-users. In 35% of frequent cell phone users, sperm motility dropped by up to half; only 9% of non-users had comparable decreases in sperm motility. | Based on questionnaire responses, 99 participants were classified as cell phone non-users; 157 had used GSM phones sporadically for 1-2 years, and 48 had used cell phones regularly for more than two years. |
| Agarwal A, Deepinder F, Sharma RK, Ranga G, Li J. 2008. Effect of cell phone usage on semen analysis in men attending infertility clinic: an observational study. Fertil Steril 89(1): 124-8. | Sperm parameters examined in 361 men undergoing infertility evaluation in 2004-2005 | Patients who used cell phones more than 4 hours a day had a 42% lower sperm count and 33% lower sperm motility than non-users. The percentage of sperm with normal morphology in high-level users was half that of non-users. Rates of normal morphology were decreased with greater levels of cell phone use. | Based on questionnaire responses, cell phone exposure was classified into four groups: no use; less than 2 hours/day; 2-4 hours/day; and more than 4 hours/day. |
| Agarwal A, Desai NR, Makker K, Varghese A, Mouradi R, Sabanegh E, et al. 2009. Effects of radiofrequency electromagnetic waves (RF-EMW) from cellular phones on human ejaculated semen: an in vitro pilot study. Fertil Steril 92(4): 1318-25. | Semen samples collected from 23 normal healthy donors and 9 infertile patients were exposed to cell phone radiation under laboratory conditions. | Semen samples exposed to cell phone radiation showed a significant drop in sperm motility (52% to 49%) and viability (59% to 52%); nearly doubled production of reactive oxygen species levels; and a decrease in total antioxidant capacity, a measure of oxidative stress. | Samples were exposed for 1 hour to radiation from a GSM cell phone in talk mode at 850 MHz. |
| De Iuliis GN, Newey RJ, King BV, Aitken RJ. 2009. Mobile phone radiation induces reactive oxygen species production and DNA damage in human spermatozoa in vitro. PLoS One 4(7): e6446. | Purified human sperm from 22 healthy donors were exposed to cell phone radiation under laboratory conditions. | Exposed sperm samples showed lower sperm motility and vitality, production of reactive oxygen species, and DNA fragmentation. At SAR of 1.0 W/kg sperm, motility decreased from 86% in unexposed sperm to 68%; vitality decreased from 89% to 65%. | Samples were exposed to 1800 MHz radiation at a range of SAR values from 0.4 W/kg to 27.5 W/kg for 16 hours at a constant temperature of 210C to rule out thermal effects. |
| Falzone N, Huyser C, Becker P, Leszczynski D, Franken DR. 2011. The effect of pulsed 900-MHz GSM mobile phone radiation on the acrosome reaction, head morphometry, and zona binding of human spermatozoa. Int J Androl 34(1): 20-6. | Purified human sperm collected from 12 healthy volunteers were exposed to cell phone radiation under laboratory conditions. | Cell phone radiation exposure appeared to affect sperm’s fertilization potential. The exposed sperm’s head area dropped by 50%. Sperm-oocyte interaction was decreased by 28% compared to unexposed controls. | Samples were exposed for 1 hour to 900 MHz GSM mobile phone radiation at a SAR of 2.0 W/kg. |
| Gutschi T, Mohamad Al-Ali B, Shamloul R, Pummer K, Trummer H. 2011. Impact of cell phone use on men’s semen parameters. Andrologia: 43(5): 312-6. | Analysis of semen samples from 2,100 men seen at an infertility clinic in 1993-2007. | 68% of the sperm from cell phone users had pathological morphology, compared to 58% of sperm from non-users. Abnormal sperm morphology was diagnosed in 45% of cell phone users versus 27.7% of non-users. | A retrospective study compared 991 cell phone users and 1,119 non-users identified via questionnaire responses. |
References
Agarwal A, Deepinder F, Sharma RK, Ranga G, Li J. 2008. Effect of cell phone usage on semen analysis in men attending infertility clinic: an observational study. Fertil Steril 89(1): 124-8.
Agarwal A, Desai NR, Makker K, Varghese A, Mouradi R, Sabanegh E, et al. 2009. Effects of radiofrequency electromagnetic waves (RF-EMW) from cellular phones on human ejaculated semen: an in vitro pilot study. Fertil Steril 92(4): 1318-25.
Aldad TS, Gan G, Gao XB, Taylor HS. 2012. Fetal radiofrequency radiation exposure from 800-1900 MHz-rated cellular telephones affects neurodevelopment and behavior in mice. Sci Rep 2: 312.
Baan R, Grosse Y, Lauby-Secretan B, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, et al. 2011. Carcinogenicity of Radiofrequency Electromagnetic Fields. Lancet Oncology 12(7): 624-26.
Davoudi M, Brossner C, Kuber W. 2002. The influence of electromagnetic waves on sperm motility [in German, “Der Einfluß elektromagnetischer Wellen auf die Spermienmotilität”]. Journal für Urologie und Urogynäkologie 9(3): 18-22.
De Iuliis GN, Newey RJ, King BV, Aitken RJ. 2009. Mobile phone radiation induces reactive oxygen species production and DNA damage in human spermatozoa in vitro. PLoS One 4(7): e6446.
Divan HA, Kheifets L, Obel C, Olsen J. 2008. Prenatal and postnatal exposure to cell phone use and behavioral problems in children. Epidemiology 19(4): 523-9.
Divan HA, Kheifets L, Obel C, Olsen J. 2012. Cell phone use and behavioral problems in young children. J Epidemiol Community Health 66(6): 524-9.
Erogul O, Oztas E, Yildirim I, Kir T, Aydur E, Komesli G, et al. 2006. Effects of electromagnetic radiation from a cellular phone on human sperm motility: an in vitro study. Arch Med Res 37(7): 840-3.
Falzone N, Huyser C, Franken DR, Leszczynski D. 2010. Mobile phone radiation does not induce pro-apoptosis effects in human spermatozoa. Radiat Res 174(2): 169-76.
Falzone N, Huyser C, Becker P, Leszczynski D, Franken DR. 2011. The effect of pulsed 900-MHz GSM mobile phone radiation on the acrosome reaction, head morphometry, and zona binding of human spermatozoa. Int J Androl 34(1): 20-6.
Fejes I, Zavaczki Z, Szollosi J, Koloszar S, Daru J, Kovacs L, et al. 2005. Is there a relationship between cell phone use and semen quality? Arch Androl 51(5): 385-93.
Gul A, Celebi H, Ugras S. 2009. The effects of microwave emitted by cellular phones on ovarian follicles in rats. Arch Gynecol Obstet 280(5): 729-33.
Gutschi T, Mohamad Al-Ali B, Shamloul R, Pummer K, Trummer H. 2011. Impact of cell phone use on men’s semen parameters. Andrologia 43(5): 312-6.
Kesari KK, Kumar S, Behari J. 2011. Effects of radiofrequency electromagnetic wave exposure from cellular phones on the reproductive pattern in male Wistar rats. Appl Biochem Biotechnol 164(4): 546-59.
Kilgallon SJ, Simmons LW. 2005. Image content influences men’s semen quality. Biol Lett 1(3): 253-5.
La Vignera S, Condorelli RA, Vicari E, D’Agata R, Calogero AE. 2012. Effects of the Exposure to Mobile Phones on Male Reproduction: A Review of the Literature. J Androl 33(3): 350-6.
Mailankot M, Kunnath AP, Jayalekshmi H, Koduru B, Valsalan R. 2009. Radiofrequency electromagnetic radiation (RF-EMR) from GSM (0.9/1.8GHz) mobile phones induces oxidative stress and reduces sperm motility in rats. Clinics (Sao Paulo) 64(6): 561-5.
Makker K, Varghese A, Desai NR, Mouradi R, Agarwal A. 2009. Cell phones: modern man’s nemesis? Reprod Biomed Online 18(1): 148-57.
Merhi ZO. 2011. Challenging cell phone impact on reproduction: a review. J Assist Reprod Genet 29(4): 293-7.
Sharlip ID, Jarow JP, Belker AM, Lipshultz LI, Sigman M, Thomas AJ, et al. 2002. Best practice policies for male infertility. Fertil Steril 77(5): 873-82.
Swan SH. 2006. Does our environment affect our fertility? Some examples to help reframe the question. Semin Reprod Med 24(3): 142-6.
Volkow ND, Tomasi D, Wang GJ, Vaska P, Fowler JS, Telang F, et al. 2011. Effects of cell phone radiofrequency signal exposure on brain glucose metabolism. Journal of the American Medical Association 305(8): 808-13.
Wdowiak A, Wdowiak L, Wiktor H. 2007. Evaluation of the effect of using mobile phones on male fertility. Ann Agric Environ Med 14(1): 169-72.
WHO (World Health Organization). 2011. IARC Classified Radiofrequency Electromagnetic Fields as Possibly Carcinogenic to Humans. Press Release # 208. 31 May 2011. Available: http://www.iarc.fr/en/media-centre/pr/2011/pdfs/pr208_E.pdf
Effect of Radiation Emitted by Wireless Devices on Male Reproductive Hormones: A Systematic Review
Maluin Sofwatul Mokhtarah, Osman Khairul, Jaffar Farah Hanan Fathihah, Ibrahim Siti Fatimah. Effect of Radiation Emitted by Wireless Devices on Male Reproductive Hormones: A Systematic Review. Frontiers in Physiology. 12:1568. 2021. doi:10.3389/fphys.2021.732420.
Abstract
Exposure to radiofrequency electromagnetic radiation (RF-EMR) from various wireless devices has increased dramatically with the advancement of technology. One of the most vulnerable organs to the RF-EMR is the testes. This is because testicular tissues are more susceptible to oxidative stress due to a high rate of cell division and mitochondrial oxygen consumption. As a result of extensive cell proliferation, replication errors occur, resulting in DNA fragmentation in the sperm. While high oxygen consumption increases the level of oxidative phosphorylation by-products (free radicals) in the mitochondria. Furthermore, due to its inability to effectively dissipate excess heat, testes are also susceptible to thermal effects from RF-EMR exposure. As a result, people are concerned about its impact on male reproductive function. This article’s aim was to review the literature on the effects of RF-EMR emitted by wireless devices on male reproductive hormones in experimental animals and humans. According to the findings of the studies, RF-EMR emitted by mobile phones and Wi-Fi devices can cause testosterone reduction. However, the effect on gonadotrophic hormones (follicle-stimulating and luteinizing hormones) is inconclusive. These findings were influenced by several factors, which can influence energy absorption and the biological effect of RF-EMR. The effect of RF-EMR in most animal and human studies appeared to be related to the duration of mobile phone use. Thus, limiting the use of wireless devices is recommended.
Conclusion
Existing animal and human data on the effect of RF-EMR emitted from wireless devices on male reproductive hormones are inconsistent and difficult to evaluate due to the heterogeneity of the study design. However, most studies are consistent with the assertion that long-term exposure to RF-EMR from mobile phones and Wi-Fi devices can disrupt male reproductive hormones, particularly testosterone. Thus, avoiding long-term and excessive use of mobile phones is advisable to reduce the detrimental effect of RF-EMR.
Open access paper: https://www.frontiersin.org/article/10.3389/fphys.2021.732420
—
Challenges on the effect of cell phone radiation on mammalian embryos and fetuses: a review of the literature
Maryam Mahaldashtian, Mohammad Ali Khalili, Fatemeh Anbari, Mohammad Seify, Manuel Belli. Challenges on the effect of cell phone radiation on mammalian embryos and fetuses: a review of the literature. Zygote. 2021 Sep 29;1-7. doi: 10.1017/S0967199421000691.
Abstract
Cell phones operate with various frequency bands and emit radiofrequency-electromagnetic radiation (RF-EMR). Concern about the possible health hazards of RF-EMR has been growing in many countries because these RF-EMR pulses may be absorbed into the body cells, directly affecting them. There are some in vitro and in vivo animal studies related to the consequences of RF-EMR exposure from cell phones on embryo development and offspring. In addition, some studies have revealed that RF-EMR from the cellular phone may decrease the rates of fertilization and embryo development, as well as the risk of developmental anomalies. Other studies have reported that it does not interfere with in vitro fertilization, intracytoplasmic sperm injection success rates, or the chromosomal aberration rate. Of course, it is unethical to study the effect of waves generated from cell phones on the forming of human embryos. Conversely, other mammals have many similarities to humans in terms of anatomy, physiology, and genetics. Therefore, in this review, we focused on the existing literature evaluating the potential effects of RF-EMR on mammalian embryonic and fetal development.
https://pubmed.ncbi.nlm.nih.gov/34583799/
Excerpts
Mobile phones are commonly placed on the lap or in pockets (Swerdlow et al., 2011), therefore exposing the genital area to RF-EMF. Germ cells are more susceptible to RF-EMF as they rapidly divide through meiosis and mitosis. EMF induces modifications in cellular levels, such as activation of voltage-gated calcium channels, formation of free radicals, protein misfolding, and DNA damage (Altun et al., 2018). In the general population, pregnant women are at specific risk of exposure to environmental RF-EMF because of their higher oxygen consumption and amniotic fluid-induced ROS production (Çiğ and Nazıroğlu, 2015) (Fig. 1). Individuals should reduce their rate of exposure to RF-EMF-emitting devices including mobile phones (Okechukwu, 2020) as electromagnetic waves enhanced the amount of oxygen free radicals in the body that led to disturbance of spermatogenesis process and variations in spermatozoa membrane, which resulted in changes in capacitation, acrosome reaction and therefore disorder in the process of spermatozoa binding to the oocyte and failure of normal fertilization both in vivo and in vitro (Fatehi et al., 2018). In addition, exposure to RF may lead to a decline in ovarian follicle reservoirs at the start of the prepubertal time (Türedi et al., 2016).
To reduce the contact with RF-EMR radiated by cell phones, people should avoid keeping their phones inside their pockets. Also, using hand-free materials and gadgets and mobile covers limits the direct exposure of cell phones to the body (Okechukwu, 2020). Also, people do not appreciate that a cell phone is a small base station and usually underrate the importance of distance between the cell phone and the body (Cousin and Siegrist, 2010). In analyzing the relationship between the distance of the cell phone antenna from the body and SAR, Hossain and colleagues reported that increasing the distance of the cell phone from the body led to the diminishing of both electric and magnetic field strength to the body, therefore reducing SAR values (Hossain et al., 2015). Furthermore, it is known that the EMF decreases with distance and magnetic induction…
Conclusion
At this time, it isn’t easy from the available animal studies to confidently document the role of RF-EMR exposure on human embryo development, both in vivo and in vitro. Further investigations with complementary techniques will be necessary to understand the mechanism of action of RF-EMR emitted by cell phones and the consequences on mammals, particularly humans.