Understanding Cancer: A Mitochondrial Metabolic Perspective for Bioelectricity Control
Cancer is one of the most complex and feared diseases of our time. Traditionally described as a condition where cell division spirals out of control, it has been the subject of intense research for decades. However, the conventional understanding that cancer is primarily a genetic disease is increasingly being challenged. This blog post explores an alternative perspective that views cancer as a mitochondrial metabolic disease, closely tied to bioelectrical control networks within the body. By understanding how these metabolic functions act as the switchboard for bioelectric control, we can gain fresh insights into managing and potentially curing this pervasive condition.
The Nature of Cancer: Cell Division Gone Awry
What is Cancer?
At its core, cancer results from cells dividing uncontrollably. Most cells in the human body exist in a differentiated, quiescent state, performing specific functions within their designated organs and tissues. These cells are highly organized, contributing to the overall health and function of the body. However, when cells in organs like the breast, bladder, colon, or lung become dysregulated in their growth, cancer begins to take root.
The Role of the Microenvironment
Cancer often starts with a chronic disruption in the cellular microenvironment. This disruption can be caused by various factors, including viral infections, chronic inflammation, or hypoxic conditions due to blocked blood vessels. These conditions do not immediately kill cells but cause a gradual loss of energy within the cell, particularly affecting the mitochondria, the powerhouse of the cell.
The Importance of Mitochondria in Bioelectrical Control
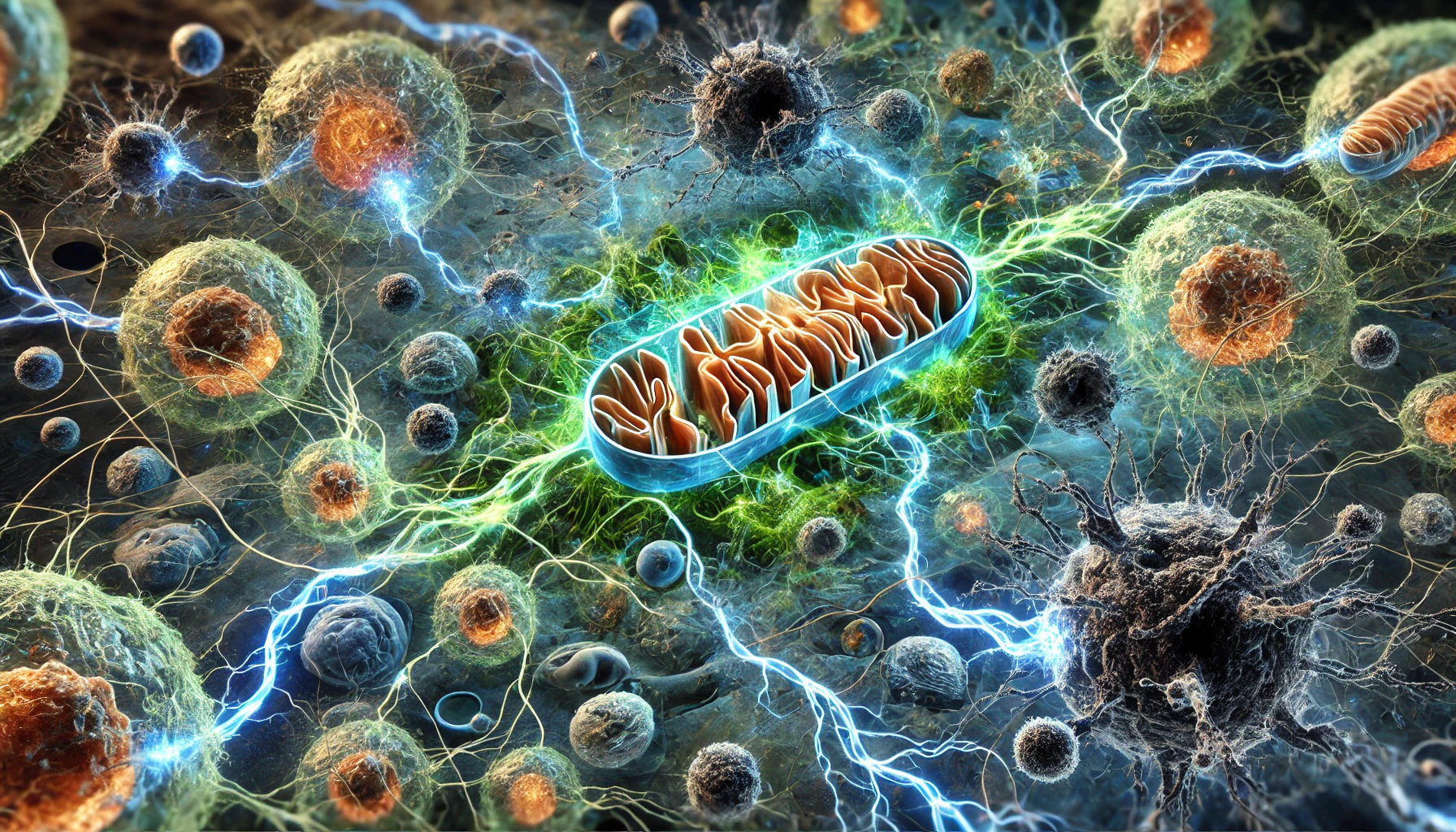
Mitochondria: The Switchboard Operators
Mitochondria are often referred to as the powerhouses of the cell, but their role extends far beyond just energy production. They are also the switchboard operators within the bioelectrical control network of the cell. Bioelectricity serves as the master control network, ensuring that all cellular activities are coordinated and that cells remain aligned with the larger goal of supporting the organism as a whole.
When mitochondria function correctly, they help maintain this bioelectric control network by generating ATP, managing calcium levels, regulating reactive oxygen species (ROS), and participating in key signaling pathways. These functions are crucial for keeping cells connected to the bioelectrical network, ensuring that they contribute to the overall health and functionality of the body. However, when mitochondrial function is compromised, this control network breaks down, leading to cellular isolation, dysregulated growth, and, ultimately, cancer.
The Metabolic Theory of Cancer
Mitochondrial Dysfunction: The Root of Cancer
The transition from healthy cell function to cancerous growth is deeply rooted in mitochondrial dysfunction. Normally, cells produce energy through oxidative phosphorylation, a highly efficient process that requires oxygen. However, when mitochondria are damaged, cells revert to fermentation, a much less efficient form of energy production that does not require oxygen.
This metabolic shift is not just a side effect of cancer; it is the driving force behind the disease. As cells become increasingly reliant on fermentation, they lose their ability to regulate growth, leading to uncontrolled cell division. This process is observed across all major types of cancer, from breast and lung cancer to melanoma and leukemia.
The Role of Glucose and Glutamine
Cancer cells thrive on glucose and glutamine, two essential fuels for fermentation. The mitochondria, in their compromised state, signal the nucleus to increase the uptake of these nutrients, fueling the rapid growth of cancer cells. This reliance on glucose and glutamine is a hallmark of cancer and provides a potential target for therapeutic intervention.
Mitochondria: The Switchboard Operators of Bioelectricity
Energy Production and Bioelectric Control
One of the primary roles of mitochondria is generating ATP through oxidative phosphorylation. This ATP acts as the energy currency for the cell, powering a vast array of cellular processes, from muscle contractions to neurotransmission. However, the production of ATP is also critical for maintaining the bioelectric potential across cell membranes, which is essential for cellular communication and the coordinated function of tissues and organs.
When mitochondrial function is disrupted, ATP production decreases, leading to a loss of bioelectric control. Without sufficient energy, cells can no longer maintain the membrane potentials necessary for proper communication, leading to a breakdown in the bioelectric network. This breakdown can cause cells to become isolated from the bioelectric signals that regulate their behavior, resulting in uncontrolled growth and the formation of tumors.
Regulating Cell Death and Maintaining Bioelectric Integrity
Mitochondria play a crucial role in programmed cell death, or apoptosis. This process is essential for removing damaged or unnecessary cells, thus maintaining cellular health and preventing diseases like cancer. Apoptosis is tightly regulated by bioelectric signals, which ensure that only the cells that are truly damaged are removed.
When mitochondria are unable to regulate apoptosis due to dysfunction, damaged cells may escape this process and continue to divide uncontrollably. This lack of regulation disrupts the bioelectric control network, allowing cancerous cells to proliferate and spread.
Calcium Homeostasis and Bioelectric Communication
Mitochondria are key regulators of intracellular calcium levels, which are critical for numerous cellular activities, including muscle contraction, neurotransmitter release, and enzyme activity. Calcium ions also play a significant role in bioelectric signaling, as they help modulate the electrical properties of cell membranes.
When mitochondrial function is impaired, calcium regulation becomes disrupted, leading to imbalances that can affect bioelectric communication. This disruption can contribute to the loss of coordinated cellular function, allowing cancerous cells to grow unchecked.
Managing ROS and Protecting the Bioelectric Network
Reactive oxygen species (ROS) are byproducts of cellular metabolism. While high levels of ROS can cause oxidative damage, mitochondria help manage this by producing and detoxifying ROS. This balance is crucial for protecting cells from oxidative stress and maintaining cellular health.
Mitochondria are also involved in maintaining the redox state of the cell, which is essential for bioelectric signaling. When mitochondria are dysfunctional, ROS levels can rise, leading to oxidative stress that damages cellular components, including those involved in bioelectric control. This damage can disrupt the bioelectric network, leading to the loss of cellular communication and the onset of cancer.
The Genetic vs. Metabolic Debate
The Genetic Theory of Cancer
The prevailing view in the medical community is that cancer is primarily a genetic disease, driven by mutations in the DNA. This theory has led to the development of targeted therapies that focus on specific genetic mutations associated with different types of cancer.
The Metabolic Theory: A Paradigm Shift
In contrast, the metabolic theory posits that cancer is a disease of mitochondrial dysfunction, where genetic mutations are a downstream effect rather than the root cause. This theory is supported by numerous studies showing that when normal mitochondria are introduced into cancer cells, their growth becomes regulated again. Conversely, when defective mitochondria are placed in healthy cells, those cells begin to exhibit cancerous behaviors.
Nuclear Transfer Experiments: A Turning Point
Nuclear transfer experiments have provided compelling evidence for the metabolic theory of cancer. These experiments involve swapping the nucleus of a cancer cell with the nucleus of a healthy cell and vice versa. The results consistently show that it is the cytoplasm, particularly the mitochondria, that dictates whether a cell behaves normally or becomes cancerous. These findings challenge the genetic model and suggest that cancer should be treated as a metabolic disease.
Implications for Cancer Treatment
Rethinking Cancer Therapies
If cancer is indeed a mitochondrial metabolic disease, then the current approach to treatment, which focuses on targeting genetic mutations, may be fundamentally flawed. Instead, therapies should aim to restore normal mitochondrial function and cut off the supply of glucose and glutamine, the key fuels for cancer cells.
The Role of Diet and Lifestyle
Diet and lifestyle play a crucial role in cancer prevention and treatment. A ketogenic diet, which is low in carbohydrates and high in fats, forces the body to rely on ketones for energy instead of glucose. Since cancer cells cannot use ketones, this dietary shift can starve them of their primary fuel source, potentially slowing or even halting cancer growth.
Non-Toxic Therapies
The metabolic theory opens the door to non-toxic therapies that target the underlying metabolic dysfunction in cancer cells. By depriving cancer cells of glucose and glutamine and enhancing mitochondrial function, it may be possible to treat cancer without the harmful side effects associated with conventional therapies like chemotherapy and radiation.
The Future of Cancer Research
Bridging the Gap Between Theory and Practice
Despite the growing body of evidence supporting the metabolic theory of cancer, it has yet to be widely adopted in clinical practice. This gap between research and treatment highlights the need for a paradigm shift in how we understand and treat cancer.
The Role of Mitochondrial Research
Future research should focus on the role of mitochondria in cancer and explore new therapies that target metabolic pathways. By improving our understanding of mitochondrial function and its impact on cell growth, we can develop more effective and less toxic treatments for cancer.
A Call to Action
The shift from viewing cancer as a genetic disease to understanding it as a mitochondrial metabolic disease has profound implications for research, treatment, and prevention. It challenges the current medical paradigm and offers a more holistic approach to managing this complex disease. The time has come for the medical community to embrace this new understanding and translate it into better outcomes for patients.
Conclusion
Cancer is not just a disease of rogue cells; it is a disease of dysfunctional mitochondria and disrupted bioelectrical communication. By rethinking our approach to cancer, focusing on the metabolic processes and bioelectrical signals that drive the disease, we can develop more effective, non-toxic treatments that target the root cause rather than just the symptoms. The metabolic theory of cancer offers a promising new direction in the fight against this devastating disease, one that has the potential to revolutionize the way we understand, treat, and ultimately cure cancer.







